Open Reduction with Internal Fixation (ORIF) Distal Humerus
Explanation of Procedure and/or Diagnosis
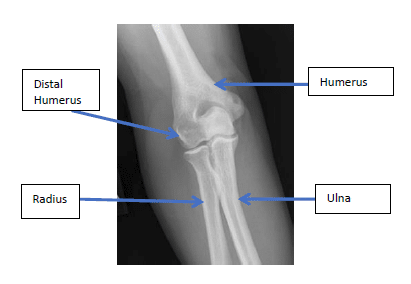 The elbow joint is made up of three bones. The lower end of the arm bone (humerus) joins with the two bones that form the forearm (radius and ulna). The ulna and radius run from the wrist to the elbow where the upper ends of these bones, the olecranon and radial head, form a hinge joint with the humerus. This is the main joint of the elbow which allows bending and straightening of the elbow. The combination of this joint along with the muscles and ligaments of the elbow allow the hand to be positioned in space for sports, physical labor and normal daily activities. The distal humerus has several complex articulations it forms, one with the ulna and the other with the radius. The distal humerus also serves as the attachment site for the two major ligaments of the elbow.
The elbow joint is made up of three bones. The lower end of the arm bone (humerus) joins with the two bones that form the forearm (radius and ulna). The ulna and radius run from the wrist to the elbow where the upper ends of these bones, the olecranon and radial head, form a hinge joint with the humerus. This is the main joint of the elbow which allows bending and straightening of the elbow. The combination of this joint along with the muscles and ligaments of the elbow allow the hand to be positioned in space for sports, physical labor and normal daily activities. The distal humerus has several complex articulations it forms, one with the ulna and the other with the radius. The distal humerus also serves as the attachment site for the two major ligaments of the elbow.
Fractures
- Severe pain in the elbow
- Difficulty moving the elbow
- Swelling of the elbow and forearm
- Deformity of the of the elbow
- Numbness or difficulty moving the hand
Most patients who have an injury severe enough to cause a distal humerus fracture are initially seen in the emergency room. The emergency room physician or your personal physician will usually recommend that you see an orthopedic surgeon within several days. Typically, your initial orthopedic visit for a distal humerus fracture will involve a history in which you describe the injury along with a limited exam of your wrist and elbow to ensure there are no other injuries including injuries to the ligaments or nerves. X-rays are necessary to determine the severity of the fracture and are usually done even if films were performed at an emergency room as the fragments can shift somewhat for the first few weeks after such an injury. CT scans are frequently necessary to better define the severity and, in many cases, help appropriately plan for any surgery.
Management of Distal Humerus Fractures
The initial management of a distal humerus fracture involves:
- Immobilization with a sling and/or splint
- “Setting” the fracture is usually not necessary except in rare instances.
- Ice and pain medication
- Visit with an orthopedic surgeon within 3-5 days to assess need for further treatment
The definitive management of your fracture will be determined by your orthopedic surgeon. The need for surgical repair of these fractures is based on the x-rays and CT scans when necessary. Because of the importance of the distal humerus in forming the elbow joint, very little displacement can be accepted and therefore, surgical management is recommended for many of these injuries. If not out of place, these can be treated non-surgically, typically with a period of immobilization in a cast of generally two to four weeks depending on the type of fracture and its stability.
Fractures in which the displacement is significant generally require surgical repair. If your fracture requires repair, your surgeon will perform an operation to reposition and hold the fracture in a more anatomic position. In some patients, bony reconstruction is not possible and replacement of the elbow may be necessary.
The elbow is considered an “unforgiving” joint, particularly with respect to distal humerus fractures. Even in the most minor distal humerus fracture and those fractures which are successfully repaired, some degree of stiffness along with development of a degree of arthritis can be expected after sustaining this type of fracture.
Non-Surgical Treatment
Many distal humerus fractures which are not out of place are often considered for surgical treatment. Because these fractures are naturally unstable, a long period of immobilization may be required for them to heal appropriately. Unfortunately, this may subsequently lead to significant and limiting stiffness. To avoid this problem alone, surgery may be considered.
There are certain fractures that are better treated non-surgically. Patient factors such as age or health may cause your surgeon to recommend a more conservative approach as well. This involves placement of a cast usually from just below the shoulder to the wrist. There is some risk of fracture shifting in the first several weeks therefore your surgeon may want to see you back several times in the first two to three weeks to ensure that the fracture position remains optimal. The frequency of these visits will depend on the type and stability of the fracture. Depending on the stability of the fracture and quality of your bone, immobilization in a cast can span three to six weeks. Once the cast is removed, typically use of a brace that allows for some motion is used for at least several weeks.
The elbow is known as an “unforgiving” joint when it comes to return of mobility after injury and even minimal fractures involving the elbow can result in some degree of stiffness. Therefore physical therapy is usually necessary as part of nonsurgical treatment of these fractures to restore full mobility and strength. Function usually becomes reasonable with minimal pain within several months after the injury. Lighter activities may be resumed within six weeks but physical activities such as sports and heavy lifting/exercise may require many months before return. Most patients continue to improve for up to a year and home exercises to improve function are usually necessary for some time even after stopping formal therapy.
Surgical Treatment
For many of these fractures, surgical repair is frequently necessary to minimize the risk of chronic pain and loss of function. Surgery is designed to reduce the amount of pain and dysfunction that otherwise would exist if a poorly positioned fracture were allowed to heal on its own. There are two primary options for surgical repair, the choice of which depends on many factors including type and severity of fracture, patient age and medical conditions, and bone quality. Reconstruction of the bone with placement of hardware is one option and in other cases, prosthetic elbow replacement is necessary. It is relatively common to consider both of these methods for a particular fracture with the ultimate decision being based on findings during the surgery.
Open Reduction with Internal Fixation (ORIF)
 Distal humerus fracture repair involves an open procedure to manipulate the fragments into an acceptable position and then fix them in place using a combination of pins and/or plates and screws. An incision is usually made over the back of the elbow and the fragments are placed in anatomic position as confirmed by an x-ray done in the operating room. This procedure may take several hours and usually requires at least an overnight stay in the hospital.
Distal humerus fracture repair involves an open procedure to manipulate the fragments into an acceptable position and then fix them in place using a combination of pins and/or plates and screws. An incision is usually made over the back of the elbow and the fragments are placed in anatomic position as confirmed by an x-ray done in the operating room. This procedure may take several hours and usually requires at least an overnight stay in the hospital.
During the surgery, often times in order to see and set the bone fragments well, the surgeon will make a small cut into the olecranon bone. Once the procedure is complete, the bone will be repaired to its original position. Additionally, often times the ulnar nerve (“funny bone” nerve) has to be moved out of the way in order to place the hardware that is needed for the procedure. This can result in some temporary numbness or tingling after surgery.
The repair is typically done with either pins or wires or a plate and screw construct. The goal of the surgery is to restore the distal humerus back to its normal anatomy as well as to securely fix the fracture so early motion can be allowed. The need for immobilization to allow healing must be balanced with the need for motion to minimize the degree of stiffness that could develop. With secure fixation, frequent motion can be allowed within several weeks of the surgery even though bony healing may take six to eight weeks.
A splint is usually placed initially, followed by a brief period of casting or your surgeon may place you directly into a brace that allows for some motion at your first postoperative visit. Physical therapy is usually necessary after splint/cast removal to restore motion and strength to the elbow. Therapy and full recovery may take months.
Total Elbow Arthroplasty (Replacement)
Generally reserved for more severe fractures or those in patients with poor bone quality (more common in older patients), elbow replacement involves removal of the bone which is too severely damaged to reconstruct and replacing it with metal and surgical-grade plastic components. This prosthesis is size-matched to the patient’s own bone. This also involves an incision over the back of the elbow and a period of splint immobilization.
Elbow replacement usually requires at least an overnight stay in the hospital. Typically, after a week or two in the splint, gentle use of the elbow is allowed. Therapy will be necessary for weeks to months after this procedure. Although motion and function generally are quite good after several months, vigorous use and heavy lifting after elbow replacement are not permissible as the prosthesis simply is not built for heavier use. Therefore, this option is generally chosen only for those patients who don’t require vigorous use of their arms or in those in whom the bone damage is so severe, replacement is the only option.
Preparing for Surgery
Prior to surgery, patients may need to see their family doctor for a medical evaluation. The purpose of this “medical clearance” evaluation is to ensure any medical conditions such as a urinary tract infection, high blood pressure, or heart disease can be detected and treated appropriately prior to your surgery. This is not always possible with fracture surgery because there is usually a narrow window of only a week or two during which the fracture needs to be treated before it begins to heal. If full medical workup is not feasible during this window, your surgeon and medical doctor will closely confer to ensure that your conditions are as stable as possible to allow for safe surgery and recovery.
NOTE: If you take aspirin, Aleve, Motrin, Plavix or Coumadin (Warfarin) or certain arthritis medications you must inform your doctor. You may need to stop these medications as soon as possible prior to your surgery. In some instances, special steps may need to be undertaken to help you safely stop these medications before your surgery.
Dentures and contact lenses cannot be worn in the operating room. Please make sure to bring your container and solutions with you to the hospital so that they may be kept safe until the completion of your surgery.
Comfortable and loose fitting clothing which can be easily put on (e.g. comfortable button down shirt or sweat shirt) will be helpful to bring for the post-operative period. The length of your hospital stay varies with some of these repairs being done as outpatient and others requiring an
overnight stay.
What to Expect at Surgery
The hospital will inform you what time you should arrive to the hospital the morning of surgery. It is essential that your orthopedic surgeon be aware of ALL the medications and supplements you are taking.
Please bring with you to the hospital a list of these medications and their dosages.
After you check in with the admissions staff, you will be taken to the pre-operative area where you will change clothes. You will meet the pre-operative nurses as well as a member of the anesthesia team. They will ask you several questions, review your medical history and examine you. The anesthesia personnel will also discuss and explain your anesthesia.
An IV will be started to provide you with fluids and medications. Special elastic stockings will also typically be applied to your legs at this time to help with your circulation during the surgery.
A member of your orthopedic surgeon’s team will also meet you in the pre-operative area to review the surgical plan and answer any questions.
Family members will have time to be with you in the pre-operative area prior to your surgery. You will be taken to the operating room where you will be transferred to a special operating table. You will meet the operating room nurses and staff who will help you get comfortable on the operating table and explain to you what steps are occurring.
Care after Surgery
After your surgery, you will arrive in the recovery room where you will be given pain medicine to keep you comfortable. You will remain in the recovery room until you have recovered completely from the anesthesia. Your arm will typically be in a splint.
To help prevent nausea during the first several days after surgery, you should slowly advance your diet from ice chips to liquids and then to regular meals. The splint is left in place until your first postoperative visit, typically a week or two after the surgery. Showering may begin on the second day as well but care must be taken to keep the splint clean and dry. Several plastic bags with tape sealant may be used. No submersion (bath or swimming) of the elbow may occur for at least four weeks after surgery.
At Home
When at home, plan to take it easy as you become increasingly independent and begin to resume your activities. You may walk as much as you like. You may drive a car when authorized by your surgeon; typically after four to six weeks. When to return to work will depend largely upon your employment duties. Check with your surgeon.
Medications
Take as prescribed. Narcotic pain medications such as Norco (hydrocodone) or oxycodone are used for severe pain. They can be taken up to every four hours as necessary. Most patients only require these medications for the first week. Once pain is better controlled, you may simply take Tylenol (acetaminophen) every four to six hours, not to exceed 3000 mg in one day. Take these medications with food. If you have any problems taking the medications, please stop them immediately and notify the clinic.
Possible Complications and Instructions
Complications:
- Bleeding
- Infection. Common signs of infection include increasing pain after surgery, increased redness around the
incision, swelling, and drainage. - Complications from anesthesia, including death
- Permanent or temporary nerve or blood vessel injury
- Failure of fixation
- Need for further surgery
- Damage to other tissues or fracture
- Loss of limb or function
- Recurrent instability is possible though uncommon
- Persistent pain
- Stiffness
- Need for manipulation, capsular release, hardware removal
- Post-traumatic arthritis
Expect to see some bruising and swelling of your arm after your fracture repair. You should advise your surgeon of any
changes around your incision. Contact your surgeon if any of the following develop:
- Drainage and/or foul odor from the incision
- Fever of 101° or greater
- Increased swelling, redness and or pain
Contact your surgeon if you develop: problems with your wound, a fever, sore throat, breathing problems, cardiac or
circulation problems or any other problems that give you concern. Also, remember to contact your surgeon if you have
any questions regarding your exercises once you have started therapy.
Do’s and Don’ts
- Do NOT use the arm to push yourself up in bed or from a chair because this requires forceful contraction of
muscles. - Do NOT overdo it. Early overuse of the arm may compromise your repair.
- Do NOT lift anything heavier than a glass of water for the first 6 weeks after surgery.
- Do NOT put your arm in any extreme position, such as straight out to the side or behind your body for the first
6 weeks after surgery. - Do ask for assistance. Your physician may be able to recommend an agency or facility if you do not have home
support.
Post-Operative Visit
Your first post-operative visit with your surgeon will typically be in 2 weeks. At this point, your stitches or staples will be
removed, your wound examined, X-rays obtained, your progress evaluated and plans for the next time interval made.
Questions
The CORE Institute is dedicated to your outcome. If any questions or concerns arise, please call The CORE Institute at 1.866.974.2673.




