Cubital Tunnel Release
Explanation of Procedure and/or Diagnosis
Anatomy
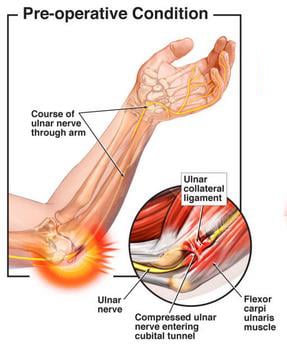
The elbow joint is made up of three bones. The lower end of the arm bone (humerus) joins with the two bones that form the forearm (radius and ulna) to form a hinge joint which allows bending and straightening of the elbow. The elbow allows the hand to be positioned in space for sports, physical labor and normal daily activities. Three major nerves cross the elbow joint, each of which contributes to control and the ability to feel in the hand.
Ulnar Nerve Irritation
The symptoms of cubital tunnel syndrome are directly related to some form of irritation of the ulnar nerve at the elbow. This is most commonly from gradual swelling of the nerve from repetitive use as well as thickening of the muscles and ligaments, which lie over the nerve, resulting in compression of the nerve as it travels through its anatomic tunnel. In some instances, irritation of the nerve can result from a severe bruise to the nerve, which likewise can cause swelling and persistent compression of the nerve under otherwise normal structures in the elbow. Symptoms of cubital tunnel syndrome can include:
- Vague elbow and forearm pain
- Partial or even full numbness in the ring and small fingers
- Clumsiness of the hand and difficulty with grip
- More noticeable symptoms at night or while driving
Generally, cubital tunnel syndrome develops gradually and frequently is present for months before people decide to inform their physician. If the symptoms are severe or do not improve with changes in activity, you will likely be asked to see an orthopedic surgeon. Typically, your initial orthopedic visit will involve learning your history in which you describe your symptoms along with an exam of your wrist and elbow to determine if and where the nerve is being irritated.
X-rays are performed to rule out the possibility that compression could be coming from abnormal bony structure at the elbow and to determine whether elbow arthritis could be involved. While the elbow is the most common place for the ulnar nerve to become irritated, it can be irritated anywhere from the neck to the wrist. To confirm the location of compression as well as to gauge the severity of the irritation, your surgeon may also recommend a nerve test be performed on your arm.
Management of Cubital Tunnel Syndrome
The initial management of ulnar nerve compression involves:
- Modifying activities to avoid those that cause nerve irritation
- Use of anti-inflammatory medications (Motrin/Advil, Aleve)
- Avoidance of pressure or resting of elbow on firm surfaces
Nonsurgical Treatment
In patients with mild, intermittent symptoms, non-operative treatment is frequently effective in relieving or markedly decreasing symptoms. Nonsurgical treatment requires some patience but can be successful in the right circumstance. In some patients, an evaluation of the workplace by an occupational therapist can be helpful to see if there are factors in the workplace which can be altered to minimize irritation of the nerve. One of the more effective approaches is use of a night splint to keep the elbow out of an excessively bent position (natural sleep position of the elbow) to minimize tension on the nerve at night. This approach does require a period of “getting used to” and tolerating the brace but can be effective if consistently used.
If these measures fail, you likely will have nerve testing performed to quantify the degree of nerve irritation. Particularly in patients who have any degree of constant numbness or weakness, earlier consideration surgical treatment is given.
Surgical Treatment
When nonsurgical measures are not effective or in patients with severe compression, surgical treatment is considered. The procedure takes some form of “decompression” or relief of pressure on the nerve. Regardless of the method used, this procedure generally does not require an overnight stay in the hospital.
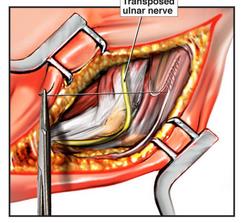
This is a procedure which is done by way of an open incision along the inside of the elbow. The structures which lie over the nerve as it courses along the elbow are opened or released. Several structures in this region are known for potentially causing pressure on the nerve and they are all released. Most of these structures are considered nonessential and little downside to releasing them has been experienced. One potential exception to this is the potential instability or tendency of the nerve to pop in and out of its groove when a complete release is performed. This is uncommon but when it occurs, can cause recurrence of nerve irritation.
In this procedure, the nerve is fully decompressed as in the above procedure. An additional step is to completely remove the nerve from its groove and create a new resting point for the nerve in the soft tissue just in front of the elbow. This requires a slightly larger incision and reduces the risk of instability of the nerve with just a simple decompression. Typically relief from numbness is experienced quickly after surgery but, depending on the degree of irritation prior to surgery, it may take months for the nerve to normalize.
Preparing for Surgery
Prior to surgery, patients may need to see their family doctor for a medical evaluation. The purpose of this “medical clearance” evaluation is to ensure any medical conditions such as a urinary tract infection, high blood pressure, or heart disease can be detected and treated appropriately prior to your surgery.
NOTE: If you take aspirin, Aleve, Motrin, Plavix or Coumadin (Warfarin) or certain arthritis medications you must inform your doctor. You may need to stop these medications as soon as possible prior to your surgery. In some instances, special steps may need to be undertaken to help you safely stop these medications before your surgery. Dentures and contact lenses cannot be worn in the operating room. Please make sure to bring your container and solutions with you to the hospital so that they may be kept safe until the completion of your surgery.
Comfortable and loose fitting clothing which can be easily put on (e.g. comfortable button down shirt or sweat shirt) will be helpful to bring for the post-operative period.
What to Expect at Surgery
The hospital or surgery center will inform you what time you should arrive to the hospital the morning of surgery. It is essential that your orthopedic surgeon be aware of ALL the medications and supplements you are taking. Please bring with you to the hospital a list of these medications and their dosages.
After you check in with the admissions staff, you will be taken to the pre-operative area where you will change clothes. You will meet the pre-operative nurses as well as a member of the anesthesia team. They will ask you several questions, review your medical history and examine you. The anesthesia personnel will also discuss and explain your anesthesia.
An IV will be started to provide you with fluids and medications. Special elastic stockings will also typically be applied to your legs at this time to help with your circulation during the surgery.
A member of your orthopedic surgeon’s team will also meet you in the pre-operative area to review the surgical plan and answer any questions.
Family members will have time to be with you in the pre-operative area prior to your surgery.
You will be taken to the operating room where you will be transferred to a special operating table. You will meet the operating room nurses and staff who will help you get comfortable on the operating table and explain to you what steps are occurring.
Care after Surgery
After your surgery, you will arrive in the recovery room where you will be given pain medicine to keep you comfortable. You will remain in the recovery room until you have recovered completely from the anesthesia. Your arm will typically be in a splint.
To help prevent nausea during the first day or so after surgery, you should slowly advance your diet from ice chips to liquids and then to regular meals. The splint is left in place until your first postoperative visit, typically a week or two after the surgery. Showering may begin on the second day as well but care must be taken to keep the splint clean and dry. Several plastic bags with tape sealant may be used. No submersion (bath or swimming) of the elbow may occur for at least four weeks after surgery.
When at home, plan to take it easy as you become increasingly independent and begin to resume your activities. You may walk as much as you like. You may drive a car when authorized by your surgeon; typically, after four to six weeks. When to return to work will depend largely upon your employment duties. Check with your surgeon.
Medications
Take as prescribed. Narcotic pain medications such as Norco (hydrocodone) or oxycodone are used for severe pain. They can be taken up to every four hours as necessary. Most patients only require these medications for the first week. Once pain is better controlled, you may simply take Tylenol (acetaminophen) every four to six hours, not to exceed 3000 mg in one day. Take these medications with food. If you have any problems taking the medications, please stop them immediately and notify the clinic.
Possible Complications
- Bleeding
- Infection. Common signs of infection include increasing pain after surgery, increased redness around the incision, swelling, and drainage.
- Complications from anesthesia, including death
- Permanent or temporary nerve or blood vessel injury
- Failure of fixation
- Need for further surgery
- Damage to other tissues or fracture
- Loss of limb or function
- Recurrent instability is possible though uncommon
Precautions and Instructions
Expect to see some bruising and swelling of your arm after your fracture repair. You should advise your surgeon of any changes around your incision. Contact your surgeon if any of the following develop:
- Drainage and/or foul odor from the incision.
- Fever of 101° or greater.
- Increasing numbness or weakness in the hand
- Increased swelling, redness and or pain
Contact your surgeon if you develop: problems with your wound, a fever, sore throat, breathing problems, cardiac or circulation problems or any other problems that give you concern. Also, remember to contact your surgeon if you have any questions regarding your exercises once you have started therapy.
Do’s and Don’ts
- Do NOT overdo it. Early overuse of the arm may compromise your result.
- Do NOT lift anything heavier than a glass of water for the first 2 weeks after surgery.
- Do ask for assistance. Your physician may be able to recommend an agency or facility if you do not have home support.
Post-Operative Visit
Your first post-operative visit with your surgeon will typically be in 2 weeks. At this point, your stitches or staples will be removed, your wound examined, your progress evaluated and plans for the next time interval made.
Questions
The CORE Institute is dedicated to your outcome. If any questions or concerns arise, please call The CORE Institute at 1.866.974.2673.




